On Thursday, Dec. 22, NYSNA nurses announced the outcome of strike authorization votes at NYC private sector hospitals with union contracts expiring Dec. 31. More than 14,000 out of 17,000 nurses at NYC private sector hospitals have completed their strike authorization votes, with 98.8 percent citywide voting in support of authorizing a strike.
Voting has completed at BronxCare, Montefiore, Mount Sinai Hospital, Mount Sinai Morningside and West, NewYork-Presbyterian, and Richmond University Medical Center. Voting is in progress at the remaining facilities, and NYSNA expects all 17,000 nurses to vote overwhelmingly in favor of authorizing a strike.
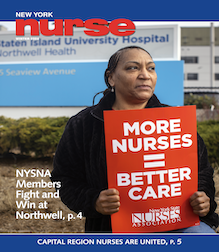
Nancy Hagans, RN, BSN, CCRN, NYSNA President and frontline nurse at Maimonides Medical Center, said: “We don’t take striking lightly. Striking is always a last resort. But we are prepared to strike if our bosses give us no other option. Nurses have been to hell and back, risking our lives to save our patients throughout the COVID-19 pandemic, sometimes without the PPE we needed to keep ourselves safe, and too often without enough staff for safe patient care. Instead of supporting us and acknowledging our work, hospital executives have been fighting against COVID nurse heroes. They’ve left us with no other choice but to move forward with voting to authorize a strike for better patient care.”
RNs have been speaking out and sounding the alarm about the short-staffing crisis puts patients at risk, especially during a tripledemic of COVID, RSV and flu. Nurses say hospitals aren’t doing enough to keep caregivers at the bedside, and instead of working with COVID nurse heroes, in some cases, are even threatening to cut their healthcare benefits.
Aretha Morgan, RN, MSN, Pediatric ER nurse at NewYork-Presbyterian, said: “Right now, we are facing a tripledemic of COVID, flu and RSV. Our pediatric ER is overflowing and short-staffed on almost all shifts. It is unbearable to see children suffer because we don’t have enough staff to provide safe patient care. And yet, NewYork-Presbyterian, which paid its CEO almost $12 million dollars in salary, bonus and perks in 2020 at the height of the pandemic, has failed to invest in hiring and retaining enough nurses.”
Approximately 17,000 NYSNA members at twelve hospitals in New York City, including some of the biggest private hospitals such as Montefiore, Mount Sinai, and NewYork-Presbyterian have contracts expiring on Dec. 31.
Ari Moma, RN, Psychiatric RN at Interfaith Medical Center in Brooklyn, said: “As a psychiatric nurse, I can tell you that the COVID-19 pandemic has pushed our patients and our nurses to their limit. Many of us were traumatized by what we saw and by the conditions we have been working under since the pandemic began. Understaffing makes everything worse. Here in Brooklyn, our safety-net hospitals, including The Brooklyn Hospital Center, Interfaith Medical Center, Kingsbrook Jewish Medical Center, Maimonides, and Wyckoff Heights Medical Center, are all fighting for fair contracts, safe staffing and respect.”
Matt Allen, RN at Mount Sinai, said: “NYSNA nurses in New York City hospitals have been sounding the alarm about chronic understaffing for years now. But at every turn–even after the devastation of COVID-19 shone a light on the problem for all to see–our hospitals have ignored nurses and continued to put profits over patient care. These so-called nonprofit hospitals lavish their executives with 7-figure salaries and bonuses. But they refuse to pay nurses fairly or protect our healthcare benefits. They pay temporary travel nurses 100% more than they pay a staff nurse, in a bottom-line driven attempt to Band-Aid over the problem that will only continue to worsen.”
Benny Mathew, RN at Montefiore in the Bronx, said: "Nurses go into this profession to help people. That’s why NYSNA nurses put forward many community proposals to assess and meet community health needs and to create a pipeline of local young people to train as the next generation of nurses. Montefiore has refused to seriously engage in bargaining over these issues. In the Emergency Department, I sometimes care for 20 patients at a time, instead of a safe standard of 3 to 6 patients. This is not safe or fair for nurses or patients. It leads to worse patient outcomes, and it increases the risk of patient death. We want safe staffing to save lives."